Scientists convert a kidney from blood type A to universal type O and implant it in a brain-dead recipient

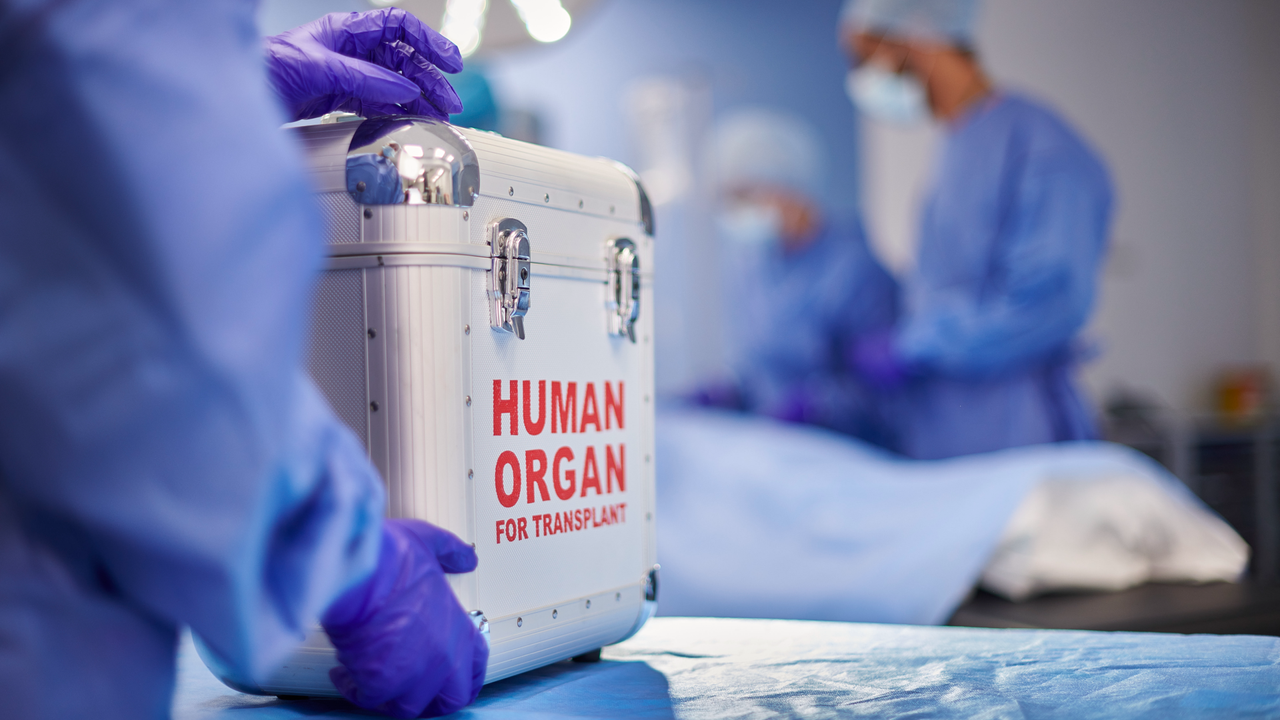
In a step towards increasing access to donor organs, scientists have converted a blood-one kidney into the blood group, and then transplanted it into a dead person from the brain.
The kidney, which had essentially been transformed into a universal transplantation organ, worked well for two days before showing signs of rejection. With refinement, this strategy could pave the way for shorter expectations on organ donors lists.
Renal transplantation is a treatment for patients with kidney disease since the 1950s. Like all organ transplants, however, it is somewhat limited by the need to match the bloody group with that of the recipient, as well as the requirement to find An organ of appropriate size which is geographically quite close to transplantation over time.
Humans have four big ones blood groups – A, B, AB and O – and the immune system of one person with a blood group can react against another type. For example, a candidate for transplantation with type O blood can only receive a rein of a type-O donor, but a person with a gay in the blood-in, B or AB can also receive a rein type O. It is because each blood group is defined by immune trigger substancescalled antigens. O Blood does not have these antigens, it can therefore be given universally, while other blood groups would trigger the immune system of a type person.
However, in the late 1980s, scientists developed a means of transplanting incompatible bodies (ABOI) – an organ of a donor with a blood group in a donor with an incompatible blood group – to recipients who needed it. But the process is demanding and takes several days. Then, in 2022, the researchers developed a Enzymes -based treatment protocol which can convert an organ into a “universal” transplant called o, or enzymatic eco converts.
“The Eco process has been demonstrated for the lungs”, co-author of the study Stephen WithersA professor emeritus of biochemistry at the University of British Columbia, told Live Science in an email. “We hope it works for all the other organs – it should!” (Earlier this year, another The research group reported the conversion of a kidney using the ecoBut they started with a blood-type-B type in their experience.)
Withers was part of the 2022 team which converted type A type A. but this team did not transplant the Eco lungs into a person in this concept proof experience. In the new study, Withers and colleagues used a type A kidney which had been deemed unsuitable for transplantation and converted it into a type-O kidney by infusing the kidney with a special liquid, which took about two hours.
“Perfusion devices and organ preservation solutions are very commonly used to keep the organs in good condition Between donation and transplantation, “Withers explained. To convert the organ, researchers have put specific enzymes into the infusion fluid which eliminated antigens from the blood group which can cause rejection.
“In this way, the organs will not be recognized and targeted by anti-A antibodies present in the recipient’s blood circulation,” said Withers. The procedure does not permanently rid the organ of problematic antigens, but it could help avoid the worst of the reaction of the immune system.
To see if the kidney could escape immediate rejection in a human, the team turned to a brain death recipient whose family has agreed to the study. The team transplanted the Eco kidney into the recipient, who wore a large amount of anti-A antibodies.
In a typical transplant, antibody therapy is given to the recipient before and after transplantation to avoid “hyperacted” rejection, which occurs quickly. But the research team wanted to test whether the creation of an Eco kidney would prevent early rejection, so they have not applied this therapy.
“We had to understand how things were growing,” said Withers. They wanted to monitor the speed at which antigens reappear in the kidney and for how long the recipient’s body could tolerate this reappearance.
The researchers found that the kidney eco worked well for two days after transplantation, without a sign of rejection. The immune responses to the new kidney appeared on the third day, that is to say that the kidney Eco began to create new antigens.
“In a real clinical transplantation, there are a number of procedures that can be applied to minimize the initial rejection mediated by antibodies, including optimized immunosuppression,” said Withers. If these methods, which are standard care in any organ transplant, are also used for Eco kidneys, this could allow longer -term tolerance of transplantation.
The conversion of organs from one blood group to another is important to increase patient access to donor organs, researchers wrote in the study. This is particularly important for “candidates of type-O transplantation, who constitute more than 50% of the waiting list and generally expect 2 to 4 years more than other blood groups,” they wrote.
Although the kidney ECO has successfully transplanted, the development of this transplantation process is still in its infancy.
“I don’t know if it will be applied universally,” said Withers. “However, this is certainly a possibility.”
This article is for information only and is not supposed to offer medical advice.