HPV vaccination drives cervical cancer rates down in both vaccinated and unvaccinated people

Human papillomavirus (HPV) vaccines can considerably reduce the rate of infections that cause cervical cancer, even in people who have not been vaccinated, reveals a new long -term study.
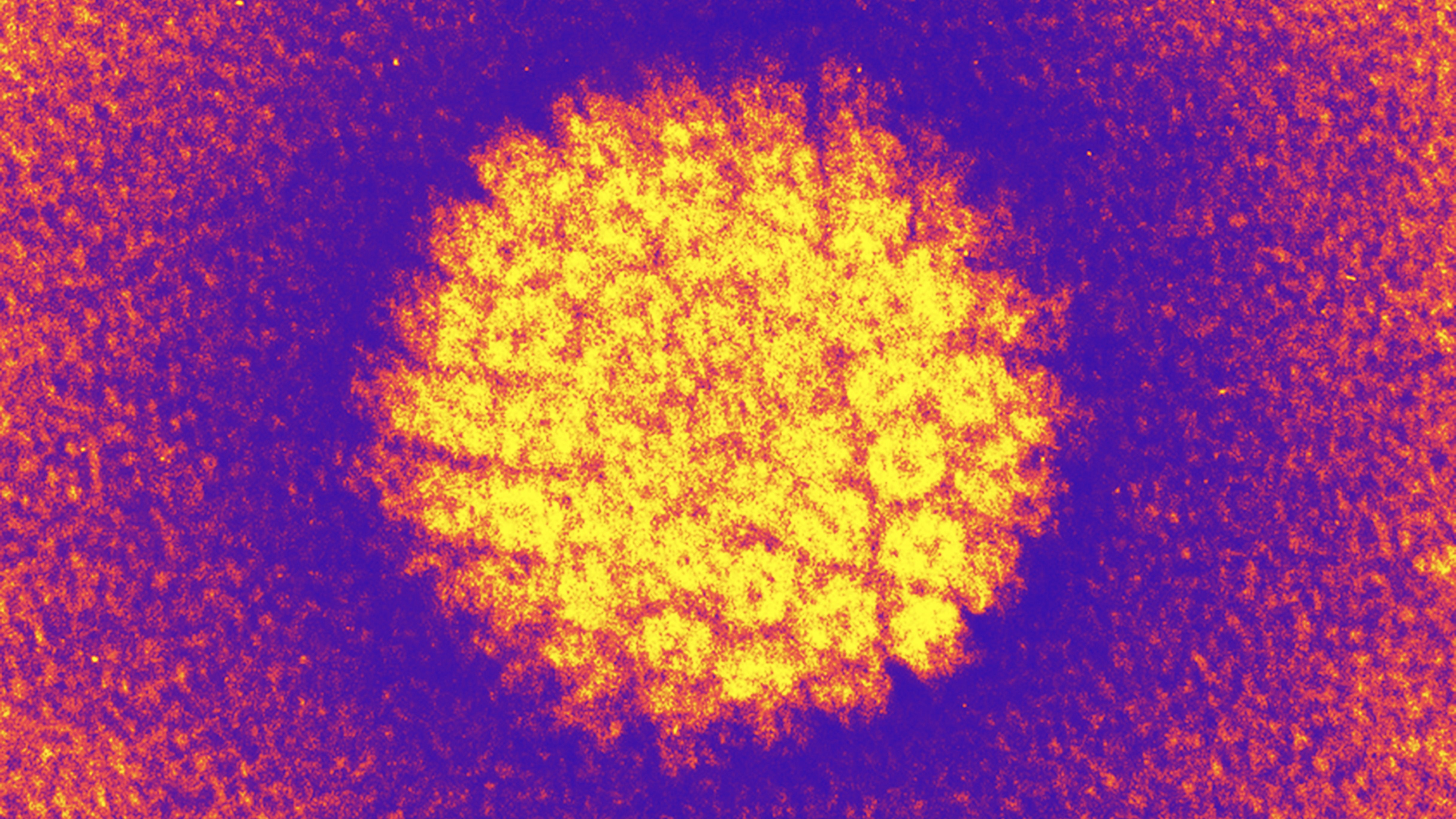
Most cases of cervical cancer are caused by high -risk HPV virusThis can cause changes to the cells that turn them cancerous. Two types of high -risk HPV are the most likely to cause cervical cancer. After the introduction of HPV vaccines in the United States, shots reduced the quantity of people testing positive for these cervical cancer viruses by a huge 98.4% in vaccinated adolescents and young women in Cincinnati, at the center of the new study. Meanwhile, in non -vaccinated people of the same age, infection rates dropped more than 71.6% during the same period.
HPV is the most common sexually transmitted infection in the world; This statistic includes both low and high risk risk strains. Although it is mainly known for its potential to cause cervical cancer, exposure to high -risk HPV can also lead to other cancers of both sexes, according to a statement published by researchers. These include those who affect the anus, head and neck.
Scientists have known for many years that HPV vaccines are very effective, significantly Reduce the rate of cervical preception in young American women and Prevent the deaths of cervical cancer. However, the new 17 -year -old study, published Monday September 29 in the journal Jama Pediatricsnoted that vaccines also reduced high -risk cervical infections in adolescent girls and young women at increased risk of HPV, even when they were not vaccinated.
Almost all sexually active people Get the HPV at some point in their lives. Infections are generally without symptoms and tend to disappear alone within two years. However, in some cases, they may persist and ultimately cause cancers.
A 2020 study published in Lancet’s global health estimated that in 2018, 690,000 cases of cancer were awarded to HPV worldwide, including 620,000 among women and 70,000 in men. College cancer represented around 80% of these cancer cases. Thus, while most people do not receive cancer due to a HPV infection, the prevalence of the virus makes it a major public health problem.
In the new study, the researchers analyzed data from six surveillance studies in Cincinnati, collected from 2006 – the year preceding the vaccine there – at 2023. The study included 2,335 adolescent girls and young women between 13 and 26 years old. They focused mainly on participants who had an increased risk of HPV because they had several sexual partners or history of sexually transmitted infection.
Several VPH vaccines have been introduced since 2006, and this study has evaluated the effectiveness of three versions: the 2 values version, which protects against HPV 16 and HPV 18, HPV responsible for more than 70% of cervical cancers; The 4 -values version, which also covers HPV 6 and HPV 11; And the 9 -values versions, which protect against five other types.
During the study period, the rate of HPV infections fell as vaccines have become available and the proportion of vaccinated participants increased, from 0% to 82%. Infections covered by the 2 -values vaccine dropped by 98.4% in vaccinated individuals, while the types of HPV remaining covered by 4 values and 9 values vaccines dropped by 94.2% and 75.7%, respectively.
The 9 -values vaccine was just as protective as vaccines with 2 values and 4 values in clinical trials, author of the main study Dr Jessica KahnProfessor of pediatrics at the Albert Einstein College of Medicine in New York, told Live Science. But the drop in virus types targeted by the 9 -values vaccine was lower in this real world scenario, because it was authorized more recently, which means that fewer participants had received at least one dose of this version at the time of the study.
Among non -vaccinated participants, HPV 16 and HPV 18 infections fell 71.6% in the studied population, while the two strains remaining covered by the 4 -values vaccine dropped by 75.8%, indicating a high degree of herd immunity. Researchers did not have enough data to effectively examine all strains covered by the new 9 -values vaccine in non -vaccinated people.
The results are good news for highly vaccinated areas, but cervical cancer rates are higher in poor countries than in the United States Globally, only 31% of adolescent girls and 8% of adolescents aged 9 to 14 have received a dose of a HPV vaccine, according to 2024 Data of the World Health OrganizationThe last available. The increase in the absorption of vaccines worldwide could have spectacular impacts.
“By expanding the adoption of this very safe and effective vaccine and ensuring access to screening and treatment, we can win one of the largest public health victories of our time: the elimination of cervical cancer,” said Kahn.
This article is for information only and is not supposed to offer medical advice.




